On the background of Find-AF 2:
Secondary stroke prophylaxis remains a challenge for neurologists. With NAVIGATE ESUS1 and RE-SPECT ESUS2, two large randomised controlled trials comparing rivaroxaban and dabigatran, respectively, with acetylsalicylic acid in ESUS patients failed to show superiority of direct oral anticoagulants in preventing stroke in the first year. In addition, the ATTICUS trial, which compared apixaban to ASA in ESUS patients, was recently stopped early on the recommendation of the Data safety monitoring board because an interim analysis showed that the planned endpoint could not be attained by the intervention.
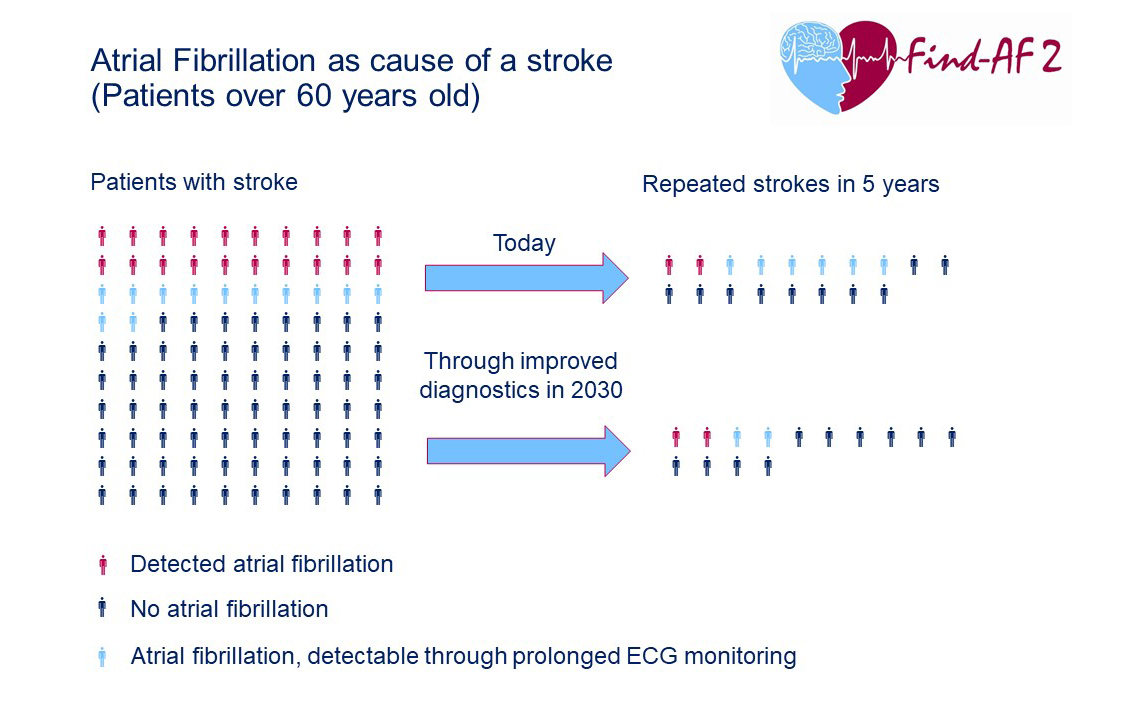
Explanation of the graph:
20 % of stroke patients have diagnosed atrial fibrillation. Another 12% have atrial fibrillation that escapes routine ECG examinations but could be detected by prolonged and intensified ECG examinations and subsequently treated by (direct) oral anticoagulation. This can significantly reduce the risk of a new stroke.
Today, out of 100 stroke patients, 18 will have a new stroke in the following five years, two of whom are patients with diagnosed and treated atrial fibrillation. Six of the 18 patients have undetected and therefore untreated atrial fibrillation. Assuming that we find and treat more previously undetected atrial fibrillation through improved and longer ECG examinations, the number of recurrent strokes could drop to 14 out of 100 patients within five years.
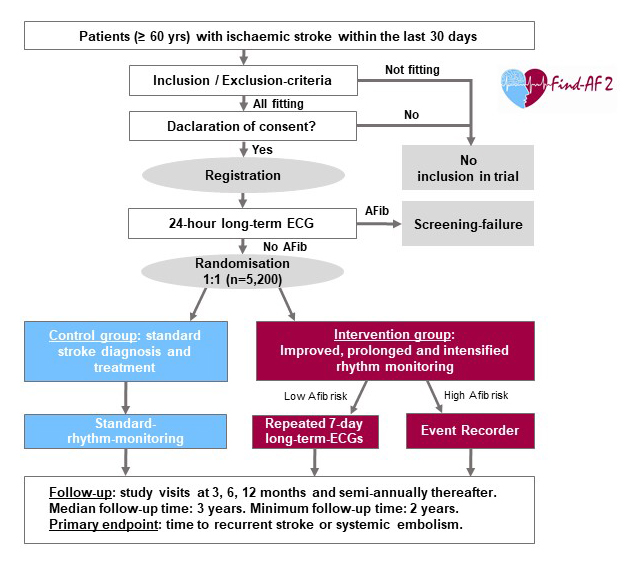
Since simple oral anticoagulation is not a viable strategy for secondary prevention in all patients with ESUS, the concept of personalised secondary stroke prevention by identifying patients with paroxysmal atrial fibrillation is coming back into focus. The EMBRACE-3, CRYSTAL-AF4 and Find-AFRANDOMISED5 trials have shown that prolonged, intensified rhythm monitoring can diagnose atrial fibrillation more frequently and earlier. It is known that atrial fibrillation leads to a switch in secondary prophylaxis from ASA to (direct) oral anticoagulants and thus to a significant risk reduction in the occurrence of a new ischaemic event.6 It is still uncertain whether the earlier start of oral anticoagulation can actually reduce the recurrence-rate of stroke.
The research group led by Prof. Rolf Wachter (Cardiology, University Hospital of Leipzig) and Prof. Klaus Gröschel (Neurology, University Hospital of Mainz) has set out to answer this important question. The Find-AF 2 study is one of the largest studies ever funded by the German Research Foundation. If the study hypothesis is confirmed with the expected risk reduction of 23 percent, an estimated 15,000 strokes per year could be prevented in Germany.
References
1. Hart RG, Sharma M, Mundl H, Kasner SE, Bangdiwala SI, Berkowitz SD, et al. Rivaroxaban for Stroke Prevention after Embolic Stroke of Undetermined Source. The New England journal of medicine. 2018;378:2191–2201.
2. Diener H-C, Sacco RL, Easton JD, Granger CB, Bernstein RA, Uchiyama S, et al. Dabigatran for Prevention of Stroke after Embolic Stroke of Undetermined Source. The New England journal of medicine. 2019;380:1906–1917.
3. Gladstone DJ, Spring M, Dorian P, Panzov V, Thorpe KE, Hall J, et al. Atrial fibrillation in patients with cryptogenic stroke. The New England journal of medicine. 2014;370:2467–2477.
4. Sanna T, Diener H-C, Passman RS, Di Lazzaro V, Bernstein RA, Morillo CA, et al. Cryptogenic stroke and underlying atrial fibrillation. The New England journal of medicine. 2014;370:2478–2486.
5. Wachter R, Gröschel K, Gelbrich G, Hamann GF, Kermer P, Liman J, et al. Holter-electrocardiogram-monitoring in patients with acute ischaemic stroke (Find-AF RANDOMISED ). An open-label randomised controlled trial. The Lancet Neurology. 2017;16:282–290.
6. Hart RG, Pearce LA, Aguilar MI. Meta-analysis. Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Annals of internal medicine. 2007;146:857–867.


